Health communication
Red Alert: How to Spot Fake Medicines in Today’s Market “Maze”?
The recent seizure of hundreds of tons of counterfeit supplements is more than just a shocking statistic—it’s a wake-up call. Your health and trust are under threat from a “maze” of low-quality products flooding the market. From prescription drugs to dietary supplements and beauty cosmetics, the line between real and fake is becoming dangerously blurred, putting consumers at serious risk.
So, how can you protect yourself and your family against this growing problem? Don’t worry—with expert tips, you can become a smart “gatekeeper” of your own health!
Today, counterfeit medicines are so sophisticated that they can even copy genuine registration numbers, batch codes, manufacturing dates, and expiration dates. In such cases, here are some practical ways to tell the difference between real and fake products:
1. Inspect packaging and appearance carefully
- Check the box and label: Packaging should be intact, with no signs of tampering, erasure, or editing.
- Read all details: Look for the drug name, batch number, manufacturing and expiry dates, registration number, and manufacturer’s name.
- Compare design elements: Pay attention to logos, fonts, and colors. If you’ve used the genuine product before, you may notice subtle differences.
- Examine the pill itself: Unusual color, size, or imprinted symbols may indicate a fake.
-

Crestor 10mg (rosuvastatin) - batch number A24236004, expiry date 7-2027 is counterfeit
-
2. Scan barcodes or QR codes – and watch for suspicious responses
- Use apps such as CheckVN (by the Ministry of Science & Technology), iCheck, or Medinsight.
- Warning signs include: links redirecting to unofficial websites, missing batch information, or odd display errors such as broken fonts or strange layouts.
3. Verify with official databases
- Visit: https://dichvucong.dav.gov.vn/congbothuoc/index
- Enter the drug’s registration number, name, and batch code to confirm whether it’s officially licensed for circulation.
-
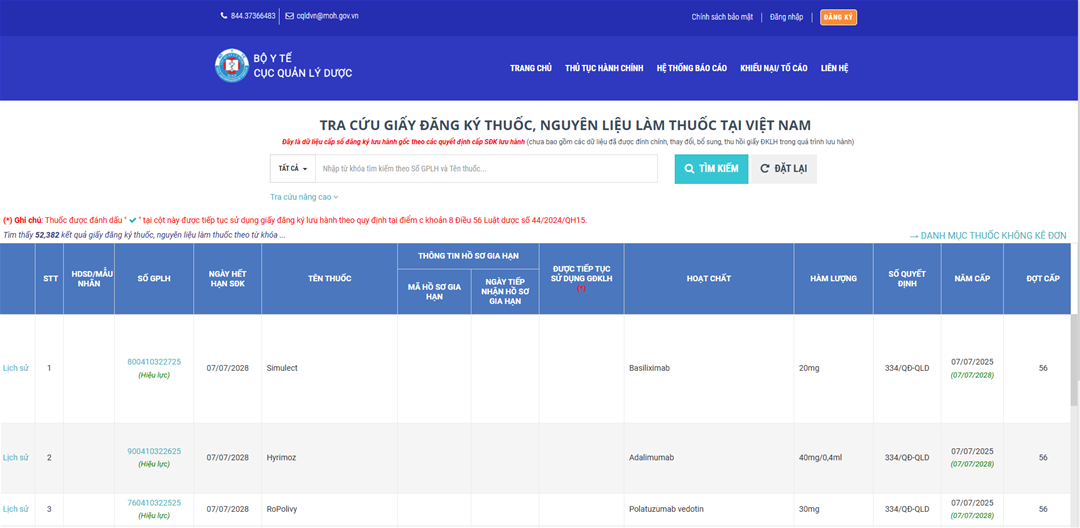
Website interface for drug registration information lookup, Ministry of Health
-
4. Use rapid testing services (via drug testing institutes)
- If still uncertain, send samples to: National Institute of Drug Quality Control (Hanoi) or your local provincial drug testing center. You can request rapid analysis to verify whether the active ingredient is authentic.
5. Choose reliable sources when buying medicine
- Only purchase from licensed pharmacies or clinics with clear signage and professional pharmacists.
- Always request an invoice or at least a receipt that includes the drug name and batch number. This can serve as proof if counterfeit products are detected.
References
- Drug Administration of Vietnam. Drug Information Lookup. Ministry of Health, Vietnam. https://dichvucong.dav.gov.vn/congbothuoc/index
- Directorate for Standards, Metrology and Quality. CheckVN Application. Ministry of Science & Technology, Vietnam. https://www.tcvn.gov.vn
- National Institute of Drug Quality Control. Drug Testing Services Information. https://www.nimqa.gov.vn
- Drug Administration of Vietnam (2023). Official Dispatch No. 1729/QLD-CL dated 24/02/2023 on counterfeit and unregistered drugs. https://www.dav.gov.vn
- Health & Life Newspaper. (May 2024). Hundreds of Tons of Counterfeit Supplements Seized in Ho Chi Minh City. https://suckhoedoisong.vn
- iCheck Corporation. iCheck App – Product Origin Verification. https://icheck.vn
MPharm. Dinh Thi Thuy Ha
MPharm. Kim Ngoc Son

